Elevated triglyceride levels can be:
• determined by genetics (primary hypertriglyceridemia) • determined by secondary causes such as metabolic syndrome, diabetes, obesity, drug reactions, poor nutrition, smoking, lack of activity and others. • determined by abnormal fat metabolism (postprandial hypertriglyceridemia)
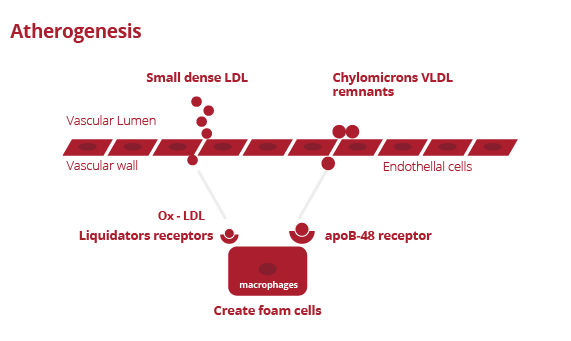
Under normal conditions, VLDL chylomicrons and VLDL remnants are metabolized and removed from circulation via special receptors. Thus, they are not converted to low-density compounds.
*Nordestgaard BG, Freiberg JJ.Clinical relevance of non-fasting and postprandial hypertriglyceridemia and remnant cholesterol.CurrVascPharmacol. 2011 May; 9(3):281-6
In case of hypertriglyceridemia (with a positive result of the Oral Fat Tolerance Test), the following changes occur:

Low-density LDL is more atherogenic than regular LDL because of:
1. Easier passage through the arterial wall.
2. Endothelial cell toxicity.
3. Promotion of the formation of thromboxane and plasminogen activator inhibitor by endothelial cells.
4. Easier oxidation.
5. Easier adhesion of glycosaminoglycans to the arterial wall.
6. Weaker association with scavenger receptors on macrophages and with LDL receptors.
*Nordestgaard BG, Freiberg JJ.Clinical relevance of non-fasting and postprandial hypertriglyceridemia and remnant cholesterol.CurrVasc Pharmacol. 2011 May; 9(3):281-6.
Low-density LDL initially binds to a specific LDL receptor that is its target, but is withdrawn from circulation by other receptors called scavenger receptors that are found on macrophages.
Conclusion:
Prolonged high plasma triglyceride levels lead to atherosclerosis by:
1. Formation of more atherogenic low-density LDL following triglyceride delivery.
2. Formation of low-density HDL, which is not as functional as regular HDL.
3. Increased levels of remnant triglycerides, which are atherogenic.
Determining fasting and non-fasting triglyceride levels cannot be the basis for diagnosing postprandial hypertriglyceridemia. Postprandial hypertriglyceridemia can only be diagnosed by performing a standardized Oral Fat Tolerance Test.
In the previous chapter we analyzed the process of atherosclerosis and its acceleration when plasma triglyceride levels are elevated. Up to now, triglyceride levels have been measured during fasting or during normal meal intake.
The instructions for measuring triglyceride levels to date were as follows:
• For fasting measurements, samples were taken after 12 to 14 hours of fasting. • For normal feeding sampling, samples were to be taken at any time without preparation or announcement, but within 8 to 14 hours of eating.
Morning samples do not show pathological postprandial triglyceride levels due to the long period of non-eating.
Fasting triglyceride levels may vary depending on:
- meal sizes
- fat content
- time arrangements (first, second meal)
- carbohydrate content
- time that has passed since a meal
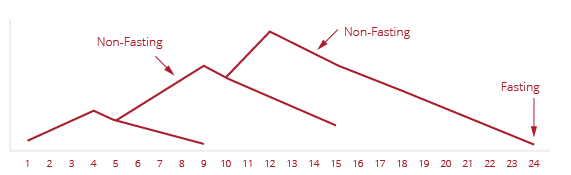
During the day we eat 3-4 meals, each with 20-40 grams of fat. As a result, the cumulative levels of triglycerides are higher than the fasting triglycerides.
Furthermore, cumulative and elevated triglyceride levels are observed after the second, third or fourth meal because the elevated triglyceride levels build on the already elevated levels from the previous meals.
Thus, elevated triglyceride levels appear throughout the day, which cannot be determined from the morning sample.
As a result, determining postprandial triglyceride levels is very important and has not been standardized until now.
Determining triglyceride levels in this way is supported by clinical studies:
• The Women’s Health Study [1]
• The Copenhagen City Heart Study [2]
• The Physicians Health Study [3]
• The Apolipoprotein-related Mortality Risk Study [4]
• The Second Northwick Park Heart Study [5]
• The Norwegian Study [6]
• The EARS II study [7]
• the ARIC study [8]
- Mora S, Rifai N, Buring JE, Ridker PM. Fasting compared with non-fasting lipids and apolipoproteins for predicting incident cardiovascular events. Circulation 2008; 118: 993-1001.
2. Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Non-fasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA 2007; 298: 299-308.
3. Stampfer MJ, Krauss RM, Ma J, et al. A prospective study of triglyceride level, low-density lipoprotein particle diameter, and risk of myocardial infarction. JAMA 1996; 276: 882-8.
4. Talmud PJ, Hawe E, Miller GJ, Humphries SE. Non fasting apolipoprotein B and triglyceride levels as a useful predictor of coronary heart disease risk in middle-aged UK men. Arterioscler Thromb Vasc Biol 2002; 22: 1918-23.
5. Waterworth DM, Talmud PJ, Bujac SR, Fisher RM, Miller GJ, Humphries SE. Contribution of apolipoprotein C-III gene variants to determination of triglyceride levels and interaction with smoking in middle-aged men. Arterioscler Thromb Vasc Biol 2000; 20:2663-9.
6. Stensvold I, Tverdal A, Urdal P, Graff-Iversen S. Non-fasting serum triglyceride concentration and mortality from coronary heart disease and any cause in middle aged Norwegian women. BMJ 1993; 307: 1318-22.
7. Tiret L, Gerdes C, Murphy MJ, Dallongeville J, Nicaud V, O’Reilly DS, Beisiegel U, De Backer G. Postprandial response to a fat tolerance test in young adults with a paternal history of premature coronary heart disease – the EARS II study (European Atherosclerosis Research Study). Eur J Clin Invest. 2000 Jul;30(7):578-85
8. Sharrett AR, Chambless LE, Heiss G, Paton CC, Patsch W. Association of postprandial triglyceride and retinyl palmitate responses with asymptomatic carotid artery atherosclerosis in middle-aged men and women. The Atherosclerosis Risk in Communities (ARIC) Study. Arterioscler Thromb Vasc Biol. 1995 Dec;15(12):2122-9.
Consumption of LIPOTEST meal enables a standardized measurement of the level of postprandial triglyceridemia.
It is worth mentioning that in 1979 Zilversmit was the first person to link the development of atherosclerosis with processes occurring after consuming a meal and emphasized the need for postprandial triglyceride tests. To date, no standardized test has been developed that would allow for obtaining a reliable result. LipiTest Control is the first test in the world that provides the possibility of a reliable assessment of postprandial lipemia.
Many clinical studies have confirmed the importance of postprandial triglyceride testing and have shown that elevated levels are observed in patients with:
• heart disease
• hypertension
• type 2 diabetes
• obesity (BMI) > 27kg/m2
• patients with metabolic syndrome
• elderly people
• menopausal women
• smokers (even with normal triglyceride levels)